Hepatitis A
- Very rare in the UK.
- Usually passed on through contaminated food and water.
- Very common in places where it is hard to access clean drinking water.
- Most people will make a full recovery without medical treatment.
- Can be more dangerous for people with a long term liver condition.
- A free and very effective vaccine is available for people at risk.

Hepatitis B
- Affects millions of people around the world.
- Passed on by blood to blood contact.
- Infections of over 6 months are called chronic hepatitis B and are usually lifelong.
- Mostly picked up at birth or as a small child.
- In some people leads to cirrhosis or liver cancer.
- Free and very effective vaccine.
- Cannot be cured, but can be controlled.

Hepatitis C
- Passed on by blood to blood contact.
- Many people won’t have symptoms for months or even years.
- Can be diagnosed and checked using blood tests.
- Free home tests available are in England.
- There is no vaccine.
- Can be easily treated. Most people have no side effects.
- If not treated, hepatitis C can be very dangerous.
Hepatitis D
- You can only get hepatitis D if you have had hepatitis B.
- You can have hepatitis B and D at the same time.
- Or you can get hepatitis D at a later date.
- The hepatitis B vaccine also protects against hepatitis D.
- Having both hepatitis B and D for a long time increases the risk of serious problems.
Hepatitis E
- Usually passed on through contaminated food or undercooked meat.
- Most people will get better in a few months.
- Can sometimes cause more serious, long term liver damage.
- People who are immunosuppressed, pregnant, or who have had a transplant are more at risk.
Tests for viral hepatitis
Get quick information about the main tests for viral hepatitis
- Antigen tests.
- Antibody tests.
- PCR tests for DNA and RNA.
You can also find more detailed information about tests on each of the condition pages.
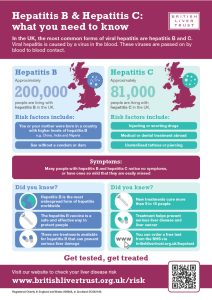
Find out moreHepatitis B and C are the leading forms of viral hepatitis in the UK, Download and share our infographic to raise awareness of the causes and risk factors to help us find more people at risk so they can get tested.
Download here